Review the study findings, “Does the Type of Cardioplegia Solution Affect Intraoperative Glucose Levels? A Propensity-Matched Analysis,” published in the March 2018 edition of the Journal of ExtraCorporeal Technology.
CLINICAL ISSUE
Cardiac surgery frequently involves the use of a heart-lung machine, requiring the heart to be temporarily and safely stopped by administering a cardioplegia (CP) solution before it is isolated from the rest of the blood circulation (“cross-clamped”).
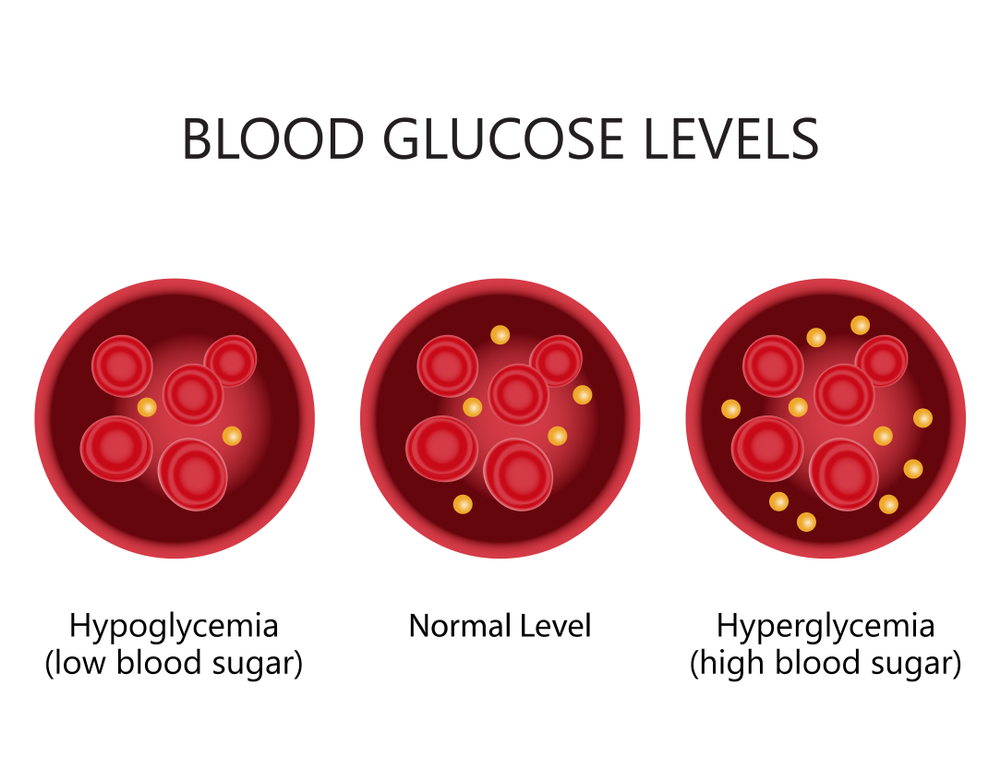
CP solutions contain varying amounts of clear fluid (“crystalloid”) as well as different electrolytes and minor additives—potentially including glucose. It is well-known that an excess of glucose in the bloodstream is associated with bad surgical outcomes, including high blood sugar (“hyperglycemia”). But, until recently, it was unknown if a glucose additive in a CP solution could affect patients’ blood glucose levels.
A research team at SpecialtyCare in Nashville, Tennessee, sought to answer that question by comparing the effect of two commonly used CP solutions on blood glucose levels in an observational study of 1,188 adult patients at 17 cardiac surgery centers across the U.S.
STUDY DESIGN
Case records for patients operated on January through October 2016 were drawn from a multi-institutional perfusion registry and included only sites using both 4:1 blood to crystalloid and del Nido cardioplegia solutions. The former contains a glucose additive, while the latter does not.
Only cases with no missing data were included. The regression analysis accounted for numerous variables that might have influenced use of one method or another, including patients’ preoperative blood glucose level and diabetes history as well as the center and physician performing the surgery.
The primary endpoint was the highest intraoperative glucose level. The secondary endpoint was maximum glucose in excess of 180 mg/dL, the trigger point for hyperglycemia.
KEY FINDINGS
In multiple ways, including bypass and cross-clamp times, the two groups were statistically indistinguishable. Meaningful differences seen among patients in the 4:1 group included a greater likelihood of having undergone coronary artery bypass graft surgery and requiring intraoperative insulin drip. Among those in the del Nido group, aortic valve and mitral valve surgery were more common, and they received a greater median volume of the CP solution.
Notably, estimated maximum intraoperative glucose for the del Nido group was 5.7 mg/dL lower (177.8 mg/dL) than for patients receiving the 4:1 solution (183.5 mg/dL) after controlling for known confounding variables. However, del Nido patients didn’t necessarily have a lower predicted probability of crossing the 180 mg/dL threshold.
EXISTING EVIDENCE
The importance of blood glucose control during surgery has been recognized since the early 1970s. An abundance of evidence since then has tied poor glucose control in diabetics undergoing cardiac surgery with a higher likelihood of wound infections, lengthy stays in the intensive care unit, and death.
Better outcomes have also been seen when blood glucose levels of surgical patients are maintained at a level no higher than 180 mg/dL, which is also the target recommended in the latest practice guidelines of the Society of Thoracic Surgeons. Hyperglycemia is associated with numerous harmful outcomes for cardiac surgery patients, including swelling in the brain, abnormal heart rhythms, and heart attacks.
The del Nido solution is relatively new to cardiac surgery, but short-term outcomes using this method have shown to be comparable to cases using traditional, blood-based cardioplegia solutions such as 4:1. In one study, patients receiving del Nido rather than blood cardioplegia were found to have a lower glucose level on leaving the operating room and required significantly less insulin.
CLINICAL EXCELLENCE IN PRACTICE
This first-time comparison of 4:1 and del Nido cardioplegia on intraoperative glucose levels revealed differences which, though clinically modest, have potentially significant implications for an institution’s bottom line. Current reimbursement guidelines of the Centers for Medicare and Medicaid Services call for a 2 percent reduction if patients’ blood glucose level exceeds 180 mg/dL within 18-24 hours post-anesthesia.
Once used mainly for pediatric surgery, del Nido is available at a growing number of cardiac surgery centers for a variety of reasons. One of its key advantages over traditional, blood-based cardioplegia is that it only needs to be administered once per hour—often once per surgery—versus every 20 minutes. Moving forward, surgery centers may want to factor into their decision-making findings of this new study suggesting del Nido may also be better at keeping patients’ glucose levels below the critical 180 mg/dL threshold triggering hyperglycemia and financial penalties.
THE RESEARCH TEAM
The study team for this research consisted of Linda B. Mongero, CCP; Eric A. Tesdahl, Ph.D.; Alfred H. Stammers, MSA, CCP; Andrew J. Stasko, MBA, CCP; and Samuel Weinstein, M.D. They are all members of the SpecialtyCare Medical Department established to maintain a quality-first focus on all clinical matters at the organization, and routinely publish in peer-reviewed journals.
LEARN MORE ABOUT PERFUSION



Comments are closed.